Connected Health
Integrating Brain and Body Mechanisms for Preventative and Personalized Health Care
Integrating Brain and Body Mechanisms for Preventative and Personalized Mental Health Care
Jyoti Mishra PhD1,
Collaborators: Sujit Dey PhD2, Dhakshin Ramanathan MD PhD1
1Neural Engineering & Translation Labs (NEATLabs), Department of Psychiatry, UC San Diego
2Center for Wireless Communication, Jacobs School of Engineering, UC San Diego
Significance. Depression, anxiety and inattention-related disorders are a leading cause of national and global disability, affecting 1-in-5 Americans and 1-in-4 humans worldwide (1, 2). In the United States alone, the socio-economic burden of these disorders is hundreds of billions of dollars every year (3). For millions of sufferers, mental illness goes undiagnosed or untreated. This is partly because the current standard of mental healthcare is based on crude subjective diagnoses, as well as one-size-fits-all, siloed interventions that are subpar in targeting the underlying problems and ridden with side effects (4).
Emerging advances in clinical and translational neuroscience research show that mental disorders stem from aberrant cognitive brain functions that systematically interact with current contextual factors of lifestyle (sleep, stress and physical activity), as well as life history, such as traumatic life experiences, and genetics (5–7). Importantly, while we cannot change our genetics and our past life histories, we can modulate our cognitive brain functions as well as contextual lifestyle factors. However, these factors are not currently utilized for clinical diagnoses/treatments. Finding feasible and scalable approaches to translate quantified evaluations of cognitive brain functions as well as daily life behaviors towards personalized diagnostics and treatments, presents a huge opportunity to design the next-generation of precision mental healthcare.
Project. In this research project, we target co-morbid mood and attention deficit disorders of depression/anxiety/ADHD, especially in young adults. These disorders typically initiate during adolescence (8), and college-age young adults are an especially vulnerable population undergoing the stress of transition to independence, while managing the load and expectations of college academics (9). This population also demonstrates apparent barriers to help-seeking including skepticism as per the effectiveness of existing treatments. Here we aim to develop an N-of-1 personalized assessment and intervention strategy for these youth, that is based on multimodal quantified measures of brain function, cognition, sleep, physical activity and stress. Using a machine learning model, these metrics will be folded into a personalized multimodal assessment & treatment for each individual. The multimodal intervention will target the most relevant neuro-cognitive and lifestyle features for that individual, which predict their mood and attention fluctuations. Such a personalized assessment and intervention approach is highly innovative and has never been studied before.
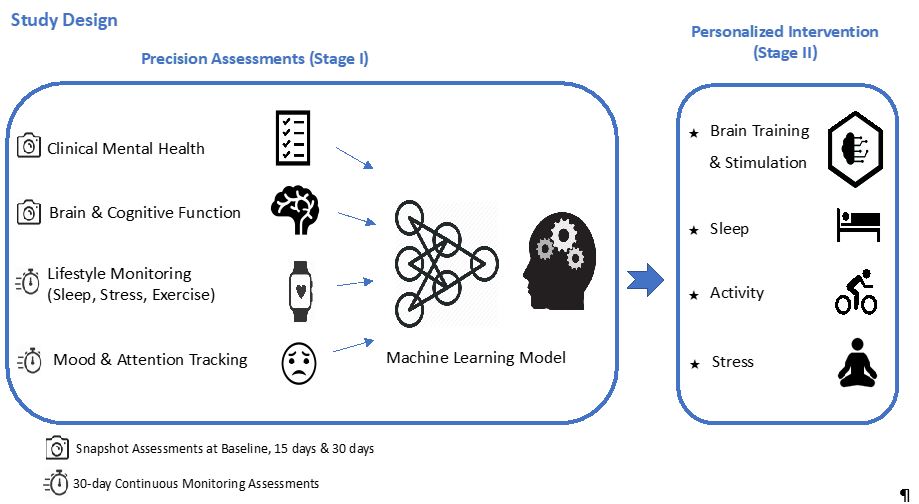
The research will be conducted in two-stages. It is important and novel in its development of quantified and personalized mental health solutions, both in terms of precision assessments in stage I, and personalized interventions in stage II.
Stage 1. Develop a precise N-of-1 assessment model predictive of an individual’s mood/attentive focus, utilizing scalable neural and cognitive function assessments as well as wearable-based tracking of sleep, stress and physical activity. In a one-month stage I study, young adults undergo snapshot assessments of neuro-cognition, using game-based cognitive modules and simultaneous mobile EEG-derived neural activity. Metrics of sleep, physical activity and stress levels are acquired over one month along with daily mood tracking data.
Stage 2. Develop a personalized multimodal intervention for each individual patient across the domains of neuro-cognition, sleep, stress and physical activity. In an two-month stage II study, we will test personalized interventions as recommended by the stage I machine learning models, where the individual focuses on the top-ranked mood/attention predictive metrics and is guided to improve them in a performance-adaptive closed-loop manner.
This study utilizes state-of-the-art, scalable assessments of brain and cognitive function, paired with longitudinal tracking of lifestyle factors (sleep, stress and physical activity) and mood and attention fluctuations. We apply machine learning models to the stage I data in each individual to determine the multidimensional (neural/cognitive/lifestyle) predictors of their depression/anxiety/attentive focus, and then transform the most predictive features into N-of-1 personalized treatment interventions in stage II (see study design below).
This study is an interdisciplinary collaboration across faculty at the UC San Diego School of Medicine Department of Psychiatry, and Jacobs School of Engineering. Principal investigator, Dr. Mishra, Assistant Professor in the department of Psychiatry, has core expertise in the clinical and translational neurosciences, and co-principal investigator, Dr. Dey, Professor of Engineering, has much expertise in developing N-of-1 predictive machine learning models using health data. Additionally, Dr. Dhakshin Ramanathan, a practicing psychiatrist at UCSD and Veterans Affairs, is a co-investigator on this project, responsible for patient monitoring and providing any medical consult needs that arise during the course of the project.
Notably, while we target mood and attention deficit disorders in young adults in this first study, our personalized approach is applicable to neuro-psychiatric mental health conditions across the human lifespan, from neurodevelopmental disorders in children, to cognitive decline in aging.
Stage I Approach. The study is recruiting 20 young adults at the UCSD Clinical & Translational Research Institute, with current symptoms of moderate depression, co-occurring with anxiety and/or attention deficit. Study participants enroll in a 30-day study, and undergo snapshot assessments at baseline, day 15, and day 30. These include:
- Subjective mental health. Individuals report on standard clinical depression/anxiety/ADHD scales (PHQ (10), GAD7 (11), ADHD RS IV (12)), and also document history of traumatic life experiences that are known to increase vulnerability to mental illness (13).
- Cognitive brain mapping. PI Mishra has developed a scalable cognitive brain mapping method that uses non-invasive, mobile & wireless EEG (electroencephalography) paired with cognitive games to rapidly assess brain activity underlying cognitive performance in core functioning domains of attention, memory, response regulation, and processing of distractions, emotions and monetary rewards (14, 15). We use these assessments to detect individual deviations from healthy cognitive brain function. This assessment can then be used to tailor a brain training/ brain stimulation based intervention strategy for eah individual.
In addition to the snapshot assessments that are completed within a one-hour research-clinic visit, the stage I study also includes continuous monitoring over 30 days:
- Lifestyle monitoring. Individuals wear a Samsung Galaxy smartwatch to objectively track lifestyle factors of sleep, physical exercise and stress (6, 16) over a one-month period. These factors are known to be modified in mood and attention-related disorders (17), and this tracking inform whether lifestyle modifications should be part of the individual’s personalized intervention.
- Mood monitoring. Using the ecological momentary assessment (EMA) method, we are asking study participants to report daily on their attentive focus, depression and anxiety, 4x per day within waking and bedtime hours (17). This continuous mood & attentive focus monitoring allows us to build a personalized model of the various factors that influence daily mood fluctuations.
Personalized Machine Learning Model. Based on all stage I assessment data from both snapshot evaluations and continuous monitoring, we are generating a machine learning model that predicts an individual’s mood/attention deficit disorder. Notably, Co-PI Dey’s team has prior experience developing such personalized models for healthcare problems such as hypertension monitoring and intervention using wearables (18). Dr. Dey and his team bring expertise in applied machine learning, which tackles real-world data mining problems by utilizing deep learning (convolutional neural networks and recurrent neural networks) and/or ensemble machine learning (random forests and gradient boosting). His team focuses on multi-modal data fusion and analytics, which is needed to efficiently utilize the various types, modes and frequency of data collected in this study. His team also has expertise in feature engineering in order to deal with limited, noisy, unaligned and irregularly sampled data usually observed in medical practice. Additionally, efficient feature selection techniques are proposed by Dr. Dey to solve the problem of overfitting in ML models. Thus, the personalized ML model in Stage I will be able to provide a precise numerical prediction of an individual’s daily fluctuating anxiety and/or depression levels, which has never been achievable before. Moreover, the ranking of input features during the feature selection process will provide personalized insight into the most important factors impacting an individual’s anxiety/depression/attention deficit, and will be used in stage II for personalized intervention recommendations.
Stage II Approach. In this stage, we will transform the outcomes of the stage I ML model, specifically the three top-ranked features that are predictive of mood for the individual into personalized multimodal intervention. The top-ranked features may be any combination of individually tailored cognitive brain training exercises or cognitive brain stimulation, specific sleep habit and/or physical exercise recommendations and/or mindfulness exercises for stress. Participants will engage in their personalized intervention plan for two-months with in-built closed-loop digital feedback on their intervention performance and progress. Clinical and neuro-cognitive assessments post-stage II will be used to quantify normalization of function, using repeated measures general linear modeling.
If successful, this personalized assessment & intervention project will be a unique advance in mental healthcare, where previously predominantly open-loop and siloed approaches have been practiced (4).
Timeline. This project has initiated as of October, 2019. The project team anticipates a three-year project period, with the stage I study completed in year 1, and stage II intervention research conducted in years 2-3.
Scientific Team & Laboratories
The project is a collaboration between co- investigators, Jyoti Mishra (Psychiatry), Sujit Dey (Engineering) and Dhakshin Ramanathan (Psychiatry) .
Dr. Mishra is an Assistant Professor in the Department of Psychiatry at UC San Diego. She is a cognitive and computational neuroscientist by training with expertise in attention, learning and brain plasticity in humans. She also has experience in innovation of digital mental health approaches & translation in neuropsychiatric populations.
Dr. Mishra directs the Neural Engineering & Translation labs (NEATLabs) located at the Altman Clinical & Translational Research Institute (ACTRI) in the department of Psychiatry. Her lab research focuses on engineering and translation of neuro-cognitive technologies that can be directly applied towards improving assessments and interventions in neuropsychiatric populations. She has contributed to R&D of closed-loop digital mental health tools, including video games, cognitive training, mindfulness-based self-regulation training, and brain computer interfaces; she holds 4 software patents and 3 software copyrights. The NEATLabs research team is multi-disciplinary including technology leadership composed of a neural engineering graduate student and a mobile applications engineer, post-doctoral fellows with training in cognitive and computational neurosciences, neuroimaging, neurophysiology and psychology, as well as undergraduate students from multiple departments across campus, such as electrical and computer engineering, bioengineering, cognitive science, and psychology. Dr. Mishra is leading the human research.
Dr. Dey is a Professor in the Department of Electrical and Computer Engineering at UCSD, where he heads the Mobile Systems Design Lab. His lab develops innovative technologies in mobile cloud computing, adaptive multimedia and networking, green computing and communications, and predictive and prescriptive analytics to enable future applications in connected health, immersive multimedia, smart cities, and smart factories. He is the Director of the Center for Wireless Communications, and the Director of the Institute for the Global Entrepreneur at UCSD. Dr. Dey leads the Connected Health program in Engineering that seeks to enable radical changes in the delivery of preventative and routine care, yielding lower care cost models with meaningful behavior changes and patient engagement. To ensure proper eco-system support and adoption of research results, he has secured early partnerships with leading healthcare providers like Kaiser Permanente and UC San Diego Health, healthcare technology leaders like Samsung Digital Health and Qualcomm Life, and big data leader Teradata. Dr. Dey and his team provides core expertise in big data prediction models, towards the development of N-of-1 personalized machine learning algorithms for this project.
Dr. Ramanathan is an attending psychiatrist at UCSD and the VA. His own research investigates neuro-cognition in animal models. In this project, he lends his psychiatry expertise towards patient monitoring and provides consults as needed during the course of the project.
References
1. Kessler RC (2007): The global burden of anxiety and mood disorders: putting the European Study of the Epidemiology of Mental Disorders (ESEMeD) findings into perspective. J Clin Psychiatry. 68 Suppl 2: 10–9.
2. Friedrich MJ (2017): Depression Is the Leading Cause of Disability Around the World. JAMA. 317: 1517.
3. Insel TR (2008): Assessing the Economic Costs of Serious Mental Illness. Am J Psychiatry. 165: 663–665.
4. Mishra J, Gazzaley A (2014): Closed-loop rehabilitation of age-related cognitive disorders. Semin Neurol. 34. doi: 10.1055/s-0034-1396011.
5. Price JL, Drevets WC (2012): Neural circuits underlying the pathophysiology of mood disorders. Trends Cogn Sci. 16: 61–71.
6. Goldstein AN, Walker MP (2014): The Role of Sleep in Emotional Brain Function. Annu Rev Clin Psychol. 10: 679–708.
7. Mullins N, Lewis CM (2017): Genetics of Depression: Progress at Last. Curr Psychiatry Rep. 19: 43.
8. Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. (2010): Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 49: 980–989.
9. Eisenberg D, Hunt J, Speer N, Zivin K (2011): Mental Health Service Utilization Among College Students in the United States. J Nerv Ment Dis. 199: 301–308.
10. Kroenke K, Spitzer RL, Williams JBW (n.d.): The PHQ-9. 46202: 606–613.
11. Spitzer RL, Kroenke K, Williams JBW, Löwe B (2006): A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med. 166: 1092–1097.
12. DuPaul G, Power T, Anastopoulos A, Reid R (1998): ADHD Rating Scale IV: checklists, norms, and clinical interpretation. New York: Guilford Press.
13. Nemeroff CB (2016): Paradise Lost: The Neurobiological and Clinical Consequences of Child Abuse and Neglect. Neuron. 89: 892–909.
14. Mishra J, Anguera JA, Gazzaley A (2016): Video Games for Neuro-Cognitive Optimization. Neuron. 90: 214–8.
15. Misra A, Ojeda A, Mishra J (2018): BrainE: a digital platform for evaluating, engaging and enhancing brain function. Regents of the University of California Copyright SD2018-816. .
16. Matta Mello Portugal E, Cevada T, Sobral Monteiro-Junior R, Teixeira Guimarães T, da Cruz Rubini E, Lattari E, et al. (2013): Neuroscience of exercise: from neurobiology mechanisms to mental health. Neuropsychobiology. 68: 1–14.
17. Merikangas KR, Swendsen J, Hickie IB, Cui L, Shou H, Merikangas AK, et al. (2019): Real-time Mobile Monitoring of the Dynamic Associations Among Motor Activity, Energy, Mood, and Sleep in Adults With Bipolar Disorder. JAMA Psychiatry. 76: 190.
18. Chiang P, Dey S (2018): Personalized Effect of Health Behavior on Blood Pressure: Machine Learning Based Prediction and Recommendation. IEEE Int Conf E-health Networking, Appl Serv.
