Connected Health
Personalized Hypertension Care using Wearables and Machine Learning
Blood pressure (BP) is one of the essential indicators of human health and can be greatly influenced by lifestyle factors (e.g., activity and sleep). However, the degree of impact of each lifestyle factor on BP is unknown and may vary significantly between individuals. Utilizing data remotely collected by home BP monitors and wearable activity trackers, we aim to use machine learning techniques to investigate the complex relationships between BP and lifestyle factors in order to provide personalized and proactive hypertension care. In addition, we investigate continuous, non-invasive BP measurement using the photoplethysmogram (PPG) sensor which has become widely accessible in wearables and medical devices. Our clinical trial with UCSD Health demonstrates prospects for reducing BP through precise lifestyle changes, either effectuated through an interactive lifestyle coach with precise recommendations.
Personalized Blood Pressure Estimation Using Photoplethysmography
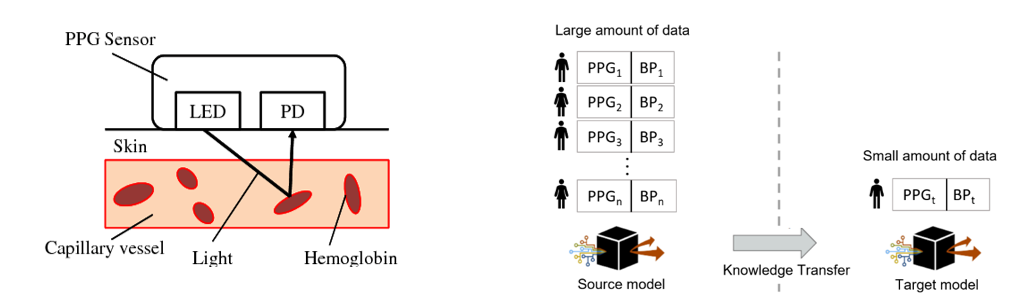
PPG principle of operation. Transfer learning overview for PPG-based BP estimation.
For accurate diagnosis and treatment of hypertension, regular BP measurement is necessary. According to the American College of Cardiology, increased at-home BP monitoring is essential for recognizing inconsistencies in measurements taken in a medical setting. Currently, the predominant device for measuring BP is a mercury sphygmomanometer which involves attaching an inflatable cuff around the upper arm. This process requires significant user effort, which limits the frequency of BP measurements and increases the chance of measurement error. The use of an arterial catheter can provide continuous BP measurement; however, it is highly invasive and impractical for daily life. With the growing trend towards digital and virtual healthcare, there is a need for an automated, continuous and accurate BP measurement technique.
In this research, we use the photoplethysmogram (PPG) sensor, which has become widely accessible in wearables and medical devices, and deep learning to enable non-invasive and continuous BP estimation. We propose a personalized deep learning approach that utilizes transfer learning in order to reduce the amount of personal PPG-BP data required from a new patient. We utilize the Multiparameter Intelligent Monitoring in Intensive Care III (MIMIC III) database in order to develop and test our method.
Personalized transfer learning approach for PPG-based BP estimation.
For future work, we will investigate a light-weight BP estimation model which can be implemented directly on a wearable device or embedded system while providing comparable performance to our current work. This will provide more real-time measurements and address concerns regarding data transmission and data privacy. While our method is developed and tested with ICU patient data, we plan to extend this approach to PPG data collected from consumer wearable devices. We will compare our personalized BP estimation models to cuff-based BP in order to further validate the accuracy.
